Advancements in spinal care are being reshaped by motion-preserving artificial discs, which offer innovative solutions to address chronic pain and spinal degeneration. Dr. Larry Davidson, a leader in minimally invasive spine surgery, recognizes that this breakthrough technology is revolutionizing the way spinal conditions are treated, improving outcomes and quality of life for patients worldwide. Unlike traditional treatments such as spinal fusion, which limit movement, artificial discs are designed to retain the spine’s natural flexibility and mobility.
The Concept of Motion Preservation in Spinal Care
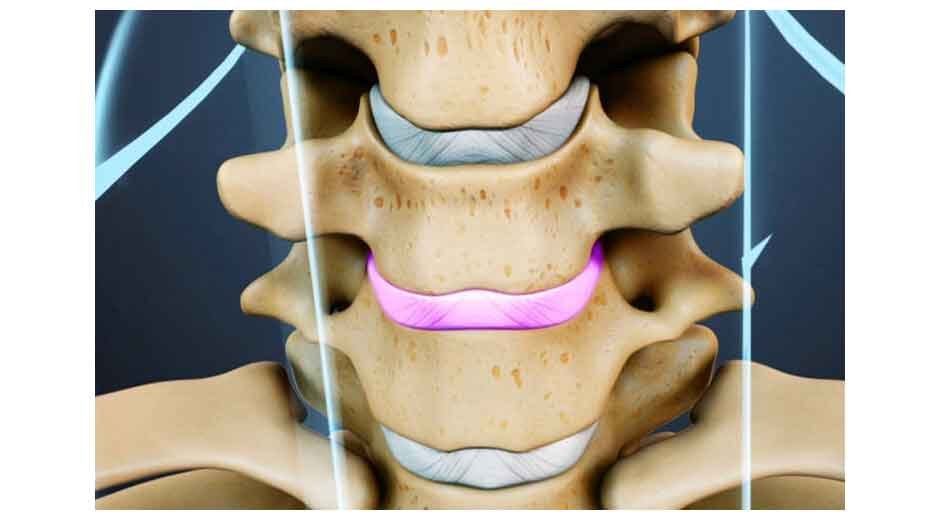
Motion-preserving artificial discs are engineered to replicate the function of a healthy spinal disc, allowing the spine to maintain its natural range of motion. These devices replace degenerated or damaged discs, alleviating pain and restoring function while minimizing stress on adjacent spinal segments.
Traditional spinal fusion, while effective for stabilizing the spine, often results in limited flexibility and increased stress on neighboring vertebrae. In contrast, artificial discs prioritize maintaining motion, reducing the long-term risks associated with adjacent segment degeneration. This emphasis on mobility offers a significant advantage, particularly for patients with active lifestyles who wish to avoid the limitations of fusion surgery.
The Benefits of Motion-Preserving Artificial Discs
One of the most significant benefits of artificial discs is their ability to retain natural movement. By mimicking the biomechanics of healthy discs, these devices allow for a smooth and unrestricted range of motion, enabling patients to perform daily activities with greater ease. Another critical advantage is the reduced stress on adjacent vertebrae. Unlike fusion surgery, which can lead to wear and tear on neighboring segments due to restricted movement, artificial discs distribute mechanical forces more naturally, minimizing the risk of further degeneration.
As Dr. Larry Davidson notes, “When considering the possibility of spinal disc replacement, a part of artificial disc surgery, the key point is proper patient selection. This adage is true with respects to all aspects of spinal surgery. The preservation of motion remains as one of the key advantages of this type of surgery.” Ensuring that the right candidates undergo artificial disc surgery is crucial, as it maximizes the benefits of motion preservation while reducing the likelihood of postoperative complications.
Recovery times are often shorter with artificial disc replacement compared to spinal fusion. The minimally invasive nature of the procedure, combined with preserved motion, allows patients to regain mobility more quickly. This contributes to an enhanced quality of life, as patients experience less postoperative pain and can return to their routines sooner. Overall, motion-preserving artificial discs provide a dynamic solution that addresses pain while promoting long-term spinal health.
Features of Modern Artificial Discs
Motion-preserving artificial discs incorporate advanced designs and materials to ensure durability, functionality and compatibility with the human body. These implants are often made from biocompatible materials such as medical-grade polyethylene and titanium alloys, which minimize the risk of adverse reactions while ensuring longevity. Their dynamic design allows for movement in all directions, including flexion, extension and rotation, closely replicating the natural mechanics of the spine.
In addition to their structural benefits, modern artificial discs can be customized to match the patient’s anatomy. This personalized approach improves the implant’s fit and functionality, optimizing surgical outcomes. These features make artificial discs a reliable option for individuals seeking to maintain their active lifestyles without compromising spinal health.
Challenges in Artificial Disc Implementation
While motion-preserving artificial discs offer numerous advantages, they are not without challenges. One of the primary limitations is patient eligibility. Not everyone is a suitable candidate for artificial disc replacement, as certain conditions such as severe arthritis, osteoporosis or extensive spinal degeneration may make the procedure less effective or riskier. Patients with multi-level spinal issues or prior surgeries may also require alternative treatment options.
Another concern is the potential for wear over time. Although artificial discs are designed for durability, prolonged use can lead to wear-related issues, sometimes necessitating revision surgery. Additionally, the procedure’s cost and limited accessibility can pose barriers for patients. The advanced technology and materials used in artificial discs often make them more expensive than traditional spinal fusion, potentially limiting availability for those without sufficient insurance coverage or resources.
Advances in Artificial Disc Technology
Advancements in artificial disc technology are enhancing the benefits of motion-preserving solutions. Hybrid designs improve strength and flexibility, while nanotechnology enhances tissue integration through nano-engineered surfaces. Smart materials adapt to spinal changes, providing greater durability and functionality and 3D printing enables personalized implants tailored to individual anatomy. These innovations are making artificial discs more reliable and effective, transforming spinal care.
Comparing Artificial Disc Replacement to Spinal Fusion
Artificial disc replacement offers a unique advantage over spinal fusion by preserving motion and reducing stress on adjacent vertebrae, a common issue with fusion. It is also less invasive, leading to shorter recovery times and reduced pain compared to the longer healing process required for spinal fusion. Both treatments have their place, with the choice depending on the patient’s condition, health and goals.
The Future of Motion-Preserving Artificial Discs
The future of spinal care is closely tied to advancements in motion-preserving artificial disc technology. Researchers are exploring ways to integrate regenerative medicine with artificial discs, combining implants with stem cells and growth factors to promote natural tissue regeneration and healing. This approach could further enhance the recovery process and extend the longevity of the implants.
Personalized medicine is also gaining momentum, with 3D printing leading the way in creating custom-fit discs that match a patient’s unique spinal anatomy. These tailored solutions offer greater precision and compatibility, reducing the risk of complications and improving outcomes. Additionally, efforts to improve the durability of artificial discs aim to address concerns about wear, ensuring that patients benefit from long-lasting solutions.
Patient Considerations for Artificial Disc Replacement
When considering artificial disc replacement, patients should collaborate with healthcare providers to assess their eligibility based on health, spinal condition severity and lifestyle goals. Selecting an experienced surgeon is vital for achieving successful outcomes. Patients should also be prepared for potential future interventions, such as revision surgery, if implant issues arise.
Motion-preserving artificial discs transform spinal care by retaining motion, reducing stress on adjacent segments and offering quicker recovery times. While challenges like patient eligibility and implant longevity persist, advancements in technology and materials are expanding their viability. As research progresses, personalized medicine and regenerative therapies promise to further enhance outcomes, enabling patients to make informed decisions and improve their quality of life.

Comments are closed.